Make Your Revenue Cycle Smooth by Denial Analysis
Making successful reimbursement payments for the medical services rendered by the American Doctors is a challenging task. The physicians are trying to make huge profits through their medical practice. For this reason, they have to make sure that the revenue cycle of their medical practice is running smoothly.
However, there are numerous barriers which can disturb the revenue cycle of the clinic. The chief reason for the decline in profits is the denial of the medical claims. Many practitioners have hired the medical billing services in the USA to prevent such denials and make successful reimbursement payments.
Fundamentally, a medical billing denial is the rejection of an insurance company to honor the claim request by the patient to pay for the treatment services rendered by a medical professional.
Medical billing denials can become a constant headache for you as it can damage the revenue, cash flow and operational efficiency of your practice. Therefore, a proper denial analysis is essential for smoothening the revenue cycle of your medical practice. For this reason, you can follow the below-mentioned practice:
Categorize the Denials
Categorizing the denials is the best way of denial analysis. The medical billing and coding experts can track, measure and report on the trends of the rejections to the medical practitioners. It will help in reducing the denial to a significant level.
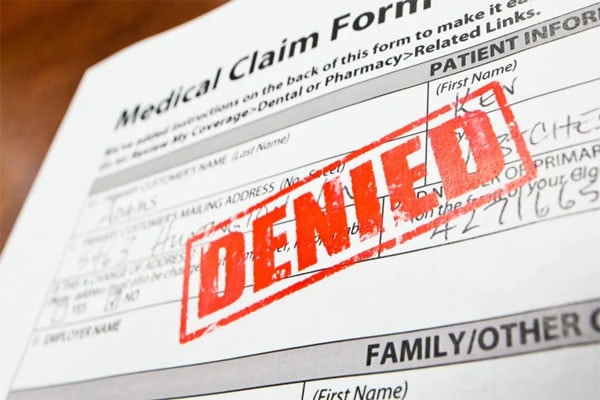
Denied Medical Claim form and denial analysis.
Image Source: Angie’s List
Technology and analytics can also assist in categorizing the denial reasons. Once you have an idea about the reasons behind the rejections, you can quickly correct them and make successful claims for payments.
Accurate Patient Data
Accuracy for patient’s data is gravely required for making successful reimbursement claims. It is necessary to enter the correct data of the patient while filling up the claim form. If the insurance company find any error in the claim regarding the patient’s information, they will reject the claim at once. The patient record is a significant source of errors and mistakes in the claims. Therefore, if the billing staff will collect the correct data of the patients upon their registration, they can avoid many denials.
Denial Prevention Mindset
The billing experts should develop a denial prevention mindset to avoid the claims rejections. For this reason, the billers should make answerable the patients for all the incomplete information. The billers should take specific steps to prevent the denials. They should improve the case management strategy which will cover the remaining deficiencies responsible for the denials.
Medical Claim Denial and Rejections.
Image Source: Capture Billing
The billers should also make accurate records of the patients. Primarily, they should concentrate on the entering the correct codes in the medical bills. The billers should not forget to comply with all the legal requirements to make a claim. Such a mindset will assist in reducing the denials and increasing the revenues.
Go for Claims Management Software
The expert billers and coders can also optimize claims management software. There is software available for keeping an eye on the whole procedure of making claims. The software helps in making successful reimbursement claims. It ensures proper functioning.
The software instantly detects if there is any missing or inaccurate information of the patient or if any code is misapplied. It helps in increasing the efficiency of the revenue cycle of the medical practice.
The medical billers and coders should adopt the tactics mentioned above to ensure a significant reduction in the claim denials. It will speed up the revenue cycle of your medical practice.
SuperbHub for more Articles and News.
Recent News
-
Duane Chapman Is Now Engaged To Girlfriend Francie Frane, Had Lost Wife 10 Months Earlier
-

Katherine Schwarzenegger Pregnant With Her First Child With Husband Chris Pratt
-

Chris Cuomo's Son Mario Tested Postive For Coronavirus
-

Kodak Black And NBA YoungBoy, Dissing One Another Via Social Media
-
Maeve Kennedy McKean, Robert F. Kennedy's Granddaughter, is Missing Along With Her Son
Entertainment
-

The Evolution of Entertainment: Online Casting Calls Redefining the Industry
-

Mamoudou Athie's Must-Watch Performances in the Movies and TV Series
-

Try These Unique Forms of Entertainment When You've Exhausted All Options
-

7 Best Movies on Netflix This Week
-

Campus Grooves: Exploring Music Festivals in American Colleges




